Case of the Month ...
Case History
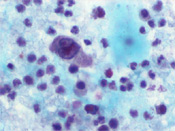
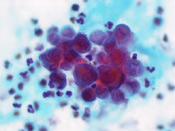
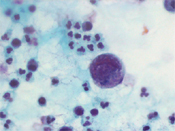
A 27 year old African-American male with a history of Hemoglobin SC disease presented with hematuria. Radiologic work-up showed bilateral enlarged kidneys, multiple areas of low attenuation in the left kidney measuring 1.8 to 4.9cm and peri-aortic lymphadenopathy. On physical examination, an enlarged left supraclavicular lymph node was noted. The voided urine showed the presence of scattered large atypical cells in a background of acute inflammation. The cells were arranged singly and in clusters and displayed high N/C ratio, coarse chromatin and prominent nucleoli. (Figure 1 - 3)
Diagnosis & Discussion
click on image for larger version
Diagnosis: Renal Medullary Carcinoma
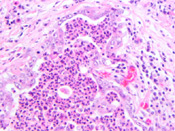
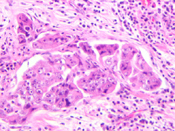
Discussion: Renal medullary carcinoma was first reported as an entity by Davis and Mostofi in 1995. 1 They described a tumor involving young male African-American patients (mean age=22 years old) with history of Sickle cell trait or hemoglobin SC disease. The tumor is located in the renal medulla and the proposed site of origin is the distal portion of the collecting ducts. The tumor frequently presents at high stage, with over 50% presenting with stage IV disease. The overall survival is short with a mean of 15 weeks in the series by Davis et al. The tumor is known to be refractory to chemotherapy and radiation therapy Histologically, these tumors have a tubulo-papillary architecture associated with marked desmoplasia and inflammatory infiltrate. (Figure 4 and 5) The cells have high N/C ratio, prominent nucleoli. Mitoses are easily identified. Sickle cells can be seen in the blood vessels in or close to the tumor. The cells in renal medullary carcinoma are immunoreactive for CAM5.2, EMA with variable expression of UEA-1, CK7 and CK 20. These same cells are not immunoreactive for 34BE12. 2, 3 Cytologically, the tumor has been described in fine needle aspiration as well as urine cytology specimens. In both types of cytology specimens, the cells present as large pleomorphic cells with granular cytoplasm, high N/C ratio, irregular nuclear borders and prominent nucleoli. Necrosis and inflammatory infiltrate are frequently seen in association with this tumor. 4-6 Gene profiling of this tumor seems to show that renal medullary carcinomas represent a tumor distinct form other types of renal carcinomas. 7
Collecting duct carcinoma represents the main histologic differential diagnosis of renal medullary carcinoma. The patients with collecting duct carcinoma are usually older and have no history of hemoglobinopathy. Inflammatory infiltrate is not common in collecting duct carcinoma. The cells in collecting duct carcinoma are immunoreactive for 34BE12 and UEA-1.
Other differential diagnosis included urothelial carcinoma, lymphoma, Wilms’ tumor, adenocarcinoma, squamous cell carcinoma, metastases and renal cell carcinoma. Urothelial carcinoma is extremely rare at this age. It occurs in an older patient population, the neoplastic cells are smaller with coarse chromatin and markedly irregular nuclear membranes. Lymphoma can occur in this age group and the most common types at this age are Burkitt’s lymphoma and diffuse large B-cell lymphoma. The lymphoid cells in these two types of lymphoma have a high N/C ratio, nucleoli are evident and the chromatin is coarse, but tumor tissue aggregates are absent. Immunocytochemistry for lymphoid markers and flow cytometry might be helpful to achieve a correct diagnosis. The patient population with Wilms’ tumor is younger (2-5 years old). Morphologically, the cells are oval and spindle with irregular nuclear membranes, uniform granular chromatin. Immunocytochemistry for WT-1 would be helpful to characterize the cells. Adenocarcinoma more commonly involves the bladder as secondary extension or metastases. It occurs in older patients and there is a previous history of malignancy. The most common adenocarcinoma to involve the bladder is prostate adenocarcinoma, which can be identified with the use of immunocytochemistry. Patients with prostate adenocarcinoma are older and do not present with hematuria. Colorectal adenocarcinoma can also involve the bladder by direct extension. Cytologically, the cells are hyperchromatic with columnar shaped nuclei and coarse chromatin. Fragments with nuclear palisading are frequently seen. Melanoma can also involve the bladder, as a primary as well as a secondary lesion. Binucleation and nuclear pseudoinclusions can be seen in melanoma. Immunohistochemistry for S100 and HMB45 can be useful in the differential diagnosis.
In summary, renal medullary carcinoma presents as a high grade epithelial malignancy, but its precise diagnosis is only possible with proper clinical correlation. Ancillary tests can be helpful in the differential diagnosis.
Acknowledgement: This case is submitted by Oscar Lin, M.D. from the Department of Pathology, Memorial Sloan Kettering Cancer Center, New York , NY
References
1. Davis CJ, Jr., Mostofi FK, Sesterhenn IA. Renal medullary carcinoma. The seventh sickle cell nephropathy. Am J Surg Pathol 1995; 19:1-11.
2. Stahlschmidt J, Cullinane C, Roberts P, Picton SV. Renal medullary carcinoma: prolonged remission with chemotherapy, immunohistochemical characterisation and evidence of bcr/abl rearrangement. Med Pediatr Oncol 1999; 33:551-7.
3. Swartz MA, Karth J, Schneider DT, Rodriguez R, Beckwith JB, Perlman EJ. Renal medullary carcinoma: clinical, pathologic, immunohistochemical, and genetic analysis with pathogenetic implications. Urology 2002; 60:1083-9.
4. Qi J, Shen PU, Rezuke WN, Currier AA, Westfall PK, Mandavilli SR. Fine needle aspiration cytology diagnosis of renal medullary carcinoma: a case report. Acta Cytol 2001; 45:735-9.
5. Larson DM, Gilstad CW, Manson GW, Henry MR. Renal medullary carcinoma: report of a case with positive urinary cytology. Diagn Cytopathol 1998; 18:276-9.
6. Hoenig JD, Husain AN, Waters BW. Pathologic quiz case: gross hematuria in a 20-year-old black woman with sickle cell trait. Renal medullary carcinoma. Arch Pathol Lab Med 2002; 126:627-9.
7. Yang XJ, Sugimura J, Tretiakova MS, et al. Gene expression profiling of renal medullary carcinoma: potential clinical relevance. Cancer 2004; 100:976-85.