Case of the Month ...
Case History
The patient was a fifty-one year old female with an approximate 10 year history of HIV infection. Her presenting complaints were pain and difficulty swallowing and occasional centralized chest pain made worse by eating. She denied having nausea, fever, vomiting, diarrhea, dark colored or bright red stools. She had been on antiretroviral therapy in the past, but was not currently taking the medications. Initial clinical workup included chest radiograph, PPD placement, and three sputum cultures. These tests yielded no evidence of a mycobacterial infection. A change in diet and trial of Diflucan lead to complete resolution of symptoms, therefore a working diagnosis of candidal esophagitis was rendered.
Three months later, the patient returned complaining of the same symptoms. An esophagogastroduodenoscopy was performed which showed diffusely ulcerated and cobblestoned mucosa involving almost the entire length of the esophagus. The patient was started on empiric herpes simplex viral therapy for esophagitis. An esophageal brush specimen was submitted to cytology, and a corresponding biopsy was sent to surgical pathology.
Diagnosis & Discussion
click on image for larger version
Figure 1
Image Figures:
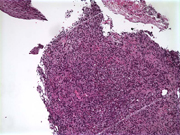
- Figure 1: fil100xa.jpg = esophageal brush, Millipore filter 100X
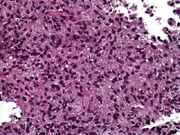
- Figure 2: esophLP.jpg = esophageal biopsy, H&E 4X
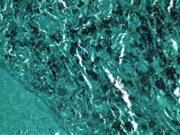
- Figure 3: esoph40x.jpg = esophageal biopsy, H&E 40X
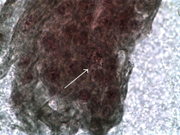
- Figure 4: gms2.jpg = esophageal biopsy, GMS 40X
Cytologic diagnosis on esophageal brushing: Intracellular fungus consistent with histoplasma capsulatum.
Histologic diagnosis on esophageal biopsy: Ulcerated squamous mucosa showing clusters of histiocytes filled with non-budding yeast compatible with Histoplasma organisms. Clinical correlation with serology/urinary antigen/culture results recommended for confirmation of fungal speciation.
Clinical Follow-up: Confirmatory laboratory test was a positive urinary histoplasma antigen.
Cytologic Findings:
- oval intracellular budding yeasts with a surrounding clear halo
- size = 2-4 microns
Discussion: Histoplasma capsulatum is a dimorphic fungus endemic to the Ohio and Mississippi River Valleys, as well as to the Caribbean. It is acquired by inhaling the microconidia found in soil/dust containing bird or bat droppings. The pathogenesis is not completely understood, however, Histoplasma yeasts are phagocytosed by macrophages. They multiply within phagolysosomes and eventually lyse the macrophage and disperse. The name “capsulatum”, originally named for what was thought to be a capsule surrounding the organism, is merely a retraction artifact seen around the organisms when inside phagolysosomes. In normal hosts, the infection is controlled by helper T-cells and cytokines that activate macrophages to kill the engulfed organisms.
Immunocompromised hosts lack cellular immune defenses, making Histoplasma a frequently encountered opportunistic pathogen. Esophageal involvement with histoplasmosis is an uncommon finding, but has been reported in the literature. The two most common scenarios are: expansion of mediastinal lymphadenopathy (with the possible complication of mediastinal fibrosis) secondarily involving the esophagus and in cases of disseminated disease. These patients usually present with dysphagia. Ulcerated mucosa or nodular lesions are typical findings in dissemination. Although our initial finding in this patient was the esophageal involvement, this patient was later found to have reactivated pulmonary disease, making the findings in the esophagus part of the disseminated process.
References:
- Henry MA, Mendes EF, Saad LH, Rodrigues PA, Goncalves I Jr. Esophageal histoplasmosis. A Case Report. Arq Gastroenterol. 1996;33(1):26-28.
- Marshall JB, Singh R, Demmy TL, Bickel JT, Everett ED. Mediastinal histoplasmosis presenting with esophageal involvement and dysphagia: case study. Dysphagia. 1995;10(1):53-58.
- Gilliland MD, Scott LD, Walker WE. Esophageal obstruction caused by mediastinal histoplasmosis: beneficial results of operation. Surgery 1984;95(1):59-62.
- Borges AS, Ferreira MS, Silvestre MT, Nishioka Sde A, Rocha A. Histoplasmosis in immunodepressed patients: study of 18 cases seen in Uberlandia, MG. Rev Soc Bras Med Trop. 1997;30(2):119-124.
- Wheat LJ, Conces D, Allen SD, Blue-Hnidy, D, Loyd J. Pulmonary Histoplasmosis Syndromes: Recognition, Diagnosis, and Management. Seminars in Respiratory and Critical Care Medicine 2004;25(2):129-143.
- Robbins & Cotran Pathologic Basis of Disease, 7th edition; Kumar, V. et al. Elsevier Saunders 2005.
Acknowledgement: *Case and photos submitted by Robyn L. Runge, MD, Marina B. Mosunjac, MD, Talaat S. Tadros, MD, and Dean Willis, SCT of Grady Memorial Hospital and Emory University Hospital, Atlanta GA.