Case of the Month ...
Case History
The patient is an 18 year-old white male who presented with a 4.5 cm right anterior cervical mass, which he first discovered 2 months ago. The mass was firm, mobile and non-tender. He complained of a sore throat and right ear pain, but denied having night sweats, fever or weight loss. The mass did not resolve with antibiotics. Fine needle aspiration of the mass was performed.
To discuss this case with your colleagues, join the PSC mailing list
Diagnosis & Discussion
click on image for larger version
Image Figs:
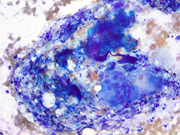
Figure 1: FNA cytology smear of parotid region mass, Diff-Quik stain, x200
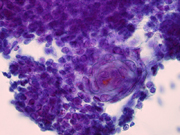
Figure 2: FNA cytology smear of parotid region mass, Papanicolaou stain, x100
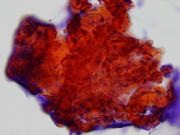
Figure 3: FNA cytology smear of parotid region mass, Papanicolaou stain, x400
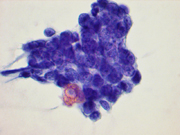
Figure 4: FNA cytology smear of parotid region mass, Papanicolaou stain, x400
Figure 5: FNA cytology smear of parotid region mass, Papanicolaou stain, x600
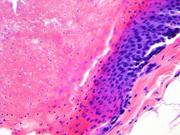
Figure 6: Surgical resection of parotid region mass, H&E stain, x200
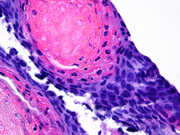
Figure 7: Surgical resection of parotid region mass, H&E stain, x400
Questions:
- What is the diagnosis?
- Pilomatrixoma
- Squamous cell carcinoma
- High grade mucoepidermoid carcinoma
- Branchial cleft cyst
- Which of the following is NOT a characteristic cytomorphologic feature of this tumor?
- Basaloid cells
- Squamous differentiation
- Calcifications
- Sharply demarcated cell clusters with peripheral palisading
- The two key cytomorphologic features of this tumor are:
- Atypical squamous cells and basaloid cells
- Anucleated squamous cells and calcium deposits
- Basaloid cells and ghost cells
- Anucleated cells and foreign body giant cells
- Which of the following is true regarding this lesion?
- It is not associated with overlying skin discoloration
- Usually presents in head, neck, face, and upper extremities of young patients
- Affects males more than females
- Preoperative clinical diagnosis is often accurate
Discussion:
Pilomatrixoma (pilomatricoma, calcifying epithelioma of Malherbe) is a tumor of hair follicle origin matrix that is almost always benign. It usually occurs in the first two decades of life and shows a female predominance. A second peak occurs in adults between 50 and 65 years of age. The most common sites for pilomatrixoma are the head, neck, face, and upper extremities. It usually presents as a painless lump and is often misdiagnosed preoperatively as an epidermoid cyst. Other preoperative clinical diagnoses include adnexal tumors, granulomatous inflammation, and malignant neoplasms including squamous cell carcinoma, small round blue cell tumors, and malignant skin appendage tumors. It may also be mistaken for a salivary gland tumor. Clinically, pilomatrixoma presents as a firm/hard nodule that may have bluish-red discoloration of the overlying skin.
Cytomorphologic findings of pilomatrixoma on fine-needle aspiration (FNA) include small to intermediate-size basaloid cells, often in dense clusters with overlapping nuclei, with high nuclear to cytoplasmic ratio and scant cytoplasm. The basaloid cells may also be arranged singly or in loosely cohesive monolayer sheets with irregular edges. Basaloid cells demonstrate fine, granular chromatin and in some cases, hyperchromatic, coarsely granular chromatin that is even in distribution. Nuclear molding has also been described in some cases. Conspicuous nucleoli may be observed. Squamous differentiation identified by the presence of cell junctions and intercellular bridging may also be seen. Squamous cells with small, dark nuclei and sparse, dense cytoplasm may be present in the center of basaloid cell clusters. Ghost or shadow cells are another important feature and are present both in clumps or as single anucleated squamous cells that often have a refractile quality. Other components observed in FNA include multinucleated giant cells, nucleated squamous cells, keratin clumps, and calcium deposition. The background is frequently hemorrhagic with amorphous debris and chronic inflammation. The two key elements in the cytologic diagnosis of pilomatrixoma are basaloid cells and ghost cells.
Histologic features of pilomatrixoma include a well-demarcated lesion comprised of basaloid cells showing squamous differentiation located at the periphery of the lesion with gradual transition to the more centrally located ghost cells. Calcium deposits, ossification, and foreign body giant cells may be present. High mitotic activity is a feature of the basaloid cells, but does not indicate malignancy. Rather, cytologic atypia, local aggressive behavior, vascular invasion, and infiltrative basaloid nodules are indicative of a malignant pilomatrixoma (pilomatrix carcinoma).
The differential diagnosis of pilomatrixoma includes adnexal cysts, parotid tumors, calcified lymph nodes, hemangioma, and malignant tumors including squamous cell carcinoma, basal cell carcinoma, Merkel cell carcinoma, and other small round blue cell tumors such as lymphoma/leukemia, Ewing’s/peripheral neuroectodermal tumor, neuroblastoma/retinoblastoma, and rhabdomyosarcoma. Mitotic figures and a background containing amorphous debris and inflammatory cells that resembles tumor necrosis are features that may be mistaken for malignancy. In contrast to squamous cell carcinoma, pilomatrixoma shows cells lacking definite malignant features and contain ghost cells. In basal cell carcinoma, the basaloid cells are arranged in tight clusters with palisading of the peripheral cells. Nucleoli are small to absent and ghost cells and multinucleated giant cells are not present. Also, mature nucleated squames are rarely seen in basal cell carcinoma.
FNA of Merkel cell tumor demonstrates a dispersed monomorphic population of atypical small cells with coarsely granular, irregular chromatin and inconspicuous nucleoli. In addition, ghost cells, nucleated squames, and multinucleated giant cells are not features of Merkel cell tumor.
Baslaoid cells may be a prominent component of some benign and malignant salivary gland tumors; however, many of these tumors (e.g., pleomorphic adenoma and adenoid cystic carcinoma) also show a characteristic stroma that is helpful to arrive at a correct diagnosis.
Answers
- a
- d
- c
- b
REFERENCES
Wang J, Cobb CJ, Martin SE, Venegas R, Wu N, Greaves TS. Pilomatrixoma: clinicopathologic study of 51 cases with emphasis on cytologic features. Diagn Cytopathol 2002;27(3):167-72.
Al-Khateeb TH, Hamasha AA. Pilomatricoma of the maxillofacial area in the northern regional Jordanian population: Report of 31 cases. J Oral Maxillofac Surg 2007;65(2):261-6.
Hwang JY, Lee SW, Lee SM. The common ultrasonographic features of pilomatricoma. J Ultrasound Med 2005;24(10):1397-402.
Julian CG, Bowers PW. A clinical review of 209 pilomatricomas. J Am Acad Dermatol 1998;39(2 Pt 1):191-5.
Kumaran N, Azmy A, Carachi R, Raine PA, Macfarlane JH, Howatson AG. Pilomatrixoma--accuracy of clinical diagnosis. J Pediatr Surg 2006;41(10):1755-8.
Lemos LB, Brauchle RW. Pilomatrixoma: a diagnostic pitfall in fine-needle aspiration biopsies. A review from a small county hospital. Ann Diagn Pathol 2004;8(3):130-6.
Lemos MM, Kindblom LG, Meis-Kindblom JM, Ryd W, Willen H. Fine-needle aspiration features of pilomatrixoma. Cancer 2001;93(4):252-6.
- Mathew S, Ali SZ. Parotid fine-needle aspiration: a cytologic study of pediatric lesions. Diagn Cytopathol 1997;17(1):8-13.
Contritbuted by:
John P. Crapanzano, M.D.
Department of Pathology
Columbia Presbyterian Medical Center
New York, NY 10032