Case of the Month ...
Case History
A 66 year old woman with history of malignant melanoma presents with an enlarging pulmonary nodule and chronic cough. The patient is a current smoker. A FNA of the pulmonary nodule was performed.
Diagnosis & Discussion
click on image for larger version
Image Figs:
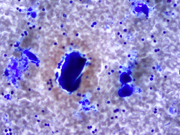
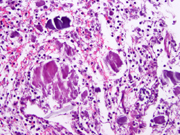
- Figure 1- FNA smears- Diff-Quik stain – 400 x.
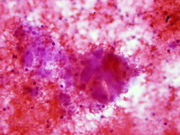
- Figure 2- FNA smear- Diff-Quik stain – 600 x.
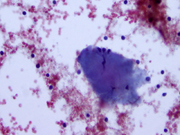
- Figure 3- FNA smear- H&E stain – 600 x.
- Figure 4- FNA smear- PAP stain – 600 x.
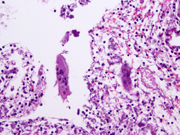
- Figure 5- Section of cell block- H&E stain- 400x.
- Figure 6- Section of cell block- H&E stain- 400x.
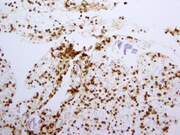
- Figure 7- Section of cell block- Immunostain for CD20- 400x.
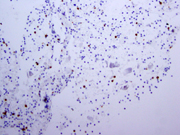
- Figure 8- Section of cell block- Immunostain for CD3- 400x .
Questions:
- What is the diagnosis?
- Granulomatous inflammation
- Chronic lymphocytic lymphoma (CLL)
- Amyloidoma
- Marginal zone lymphoma (MALT) with associated amyloid deposition.
- What is the most common primary pulmonary lymphoma?
- MALT lymphoma
- Diffuse large B-cell lymphoma
- Hodgkins Lymphoma
- Chronic lymphocytic lymphoma
- What other pathological entities can be associated with this lymphoma?
- Squamous cell carcinoma and granuloma
- Amyloid and granulomatous reaction
- Granuloma and large cell lymphoma
- EBV infection and plasmacytoma
- What is the best immunoprofile to diagnose this lymphoma?
- CD20, CD5, CD21 positive cells.
- CD20, BCL-2, BCL-6, CD10 positive cells
- Mixture of CD20 and CD3 positive cells
- CD20, BCL2 positive cells.
Discussion: Primary lymphoma of lung are defined as monoclonal lymphoid proliferations that affect one or both lungs or bronchi in an individual who has no evidence of extrapulmonary tumor at time of diagnosis or for three months thereafter 1 . Primary pulmonary lymphomas represent only 0.5-1% of primary malignancies of the lung 1, 2 . Most of the primary pulmonary lymphomas are low-grade. 1-3 .
MALT lymphomas are the most common primary pulmonary lymphoma. This tumor is more commonly seen in woman in the sixth decade of life. One-third of the patients have asymptomatic solitary nodules or masses, usually less than 5 cm in diameter 3-5 . Multiple nodules can be seen; Symptoms include cough, dyspnea, and hemoptysis and chest pain 3, 4 . A minority has constitutional symptoms such as fever, weight loss and night sweats.
Recurrences occur in a high proportion of patients nearly 50% after 2 years 1 . They most often involve lung or other mucosal sites such as gastrointestinal tract or salivary gland. The prognosis of MALT lymphomas is generally good, with 5- and 10-year survivals of 84-88% 3 . Surgical management with clean margin is the best therapeutic modality for localized tumors. Chemotherapy can be used for diffuse or bilateral involvement of the lung or when there is concomitant extrapulmonary disease.
The cytological diagnosis of MALT lymphoma can be challenging because of overlapping criteria with reactive lymphoid hyperplasia 6 . The diagnosis of pulmonary lymphoma should be suspect when there is a predominant lymphoid population on the smears. The neoplastic cells like most low-grade lymphomas are represented by a predominance of intermediate-sized population of lymphocytes in a background of mild inflammatory (plasma cells) infiltrate and some small and activated lymphocytes 6, 7 . The diagnosis can be made with the use of flow-cytometry and/or immunocytology. In the current case, the neoplastic lymphocytes were positive for CD20 and bcl-2, whereas negative for bcl-6, CD10, cyclin-D1, and CD 23. Admixed T-lymphocytes were positive for CD5 and CD3. In case of very limited material, when a complete panel of immuno markers for low-grade lymphoma can not be done, stains for CD20 and CD3 will show an over representation of B-cells in the cytologic material, which should raise suspicion for a neoplastic process. In out case, the neoplastic cells were restricted for lambda light chain. However, it is often difficult to demonstrate light chain restriction by immunohistochemical stains in MALT lymphomas. In these cases, molecular studies can show clonal rearrangement of the immunoglobulin heavy chain gene 2, 8 in about 60-70% of the tumors. Molecular tests can be performed in cell block preparation.
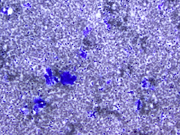
The amorphous material that was so abundant on the smears was positive for amyloid by Congo Red stain performed on sections of the cell block. The association of MALT lymphoma and amyloid deposition is rare, but a search for lymphoma should be carried out any time amyloid deposition is diagnosed in the lung 9, 10 .
Answers
- d
- a
- b
- d
REFERENCES
1. Cadranel J, Wislez M, Antoine M. Primary pulmonary lymphoma. Eur Respir J 2002. 20:75-762.
2. Begueret H, Vergier B, Parrens M, et al. Primary lung small B-cell lymphoma versus lymphoid hyperplasia. Am J Surg Pathol 2002. 26:76-81.
3. Kurtin PJ, Myers JL, Adlakha H, et al. Pathology and clinical features of primary pulmonary extranodal marginal zone B-cell lymphoma of MALT type. Am J Surg Pathol 2001. 25:997-1008.
4. Li G, Hansmann M-L, Zwingers T, et al. Primary lymphoma of the lung: morphological, immunohistochemical and clinical features. Histopathology 1990. 16:519-531.
5. Fiche M, Caprons F, Berger F, et al. Primary pulmonary non-Hodgkin's lymphomas. Histopathology 1995. 26:529-37.
6. Crapanzano JP, Lin O. Cytologic findings of marginal zone lymphoma. Cancer. 2003. 99:301-9.
7. Chhieng DC, Cohen JM, Cangiarella JF. Cytology and immunophenotyping of low-grade and intermediate-grade B-cell non-Hodgkin's lymphomas with a predominant small-cell component: a study of 56 cases. Diagn Cytopathol. 2001. 24:90-7.
8. Wotherspoon A, Pan L, Diss T, et al. A genotypic study of low grade B-cell lymphomas, including lymphomas of mucosa associated lymphoid tissue (MALT). J Pathol 1990. 162:135-140.
9. Lim JK, Lacey MQ, Kurtin PJ et al. Pulmonary marginal zone lymphoma of MALT Type as a cause of localized amyloidosis. J Clin Pathol 2001.54:642-6.
10- Satani T, Yokose T, Kaburagi T et al. Amyloid deposition in primary marginal zone B-cell lymphoma of mucosa-associated tissue. Pathol Int. 2007.57:746-50.
Case contributed by Andre L. Moreira, M.D. PhD
Memorial Sloan Kettering Cancer Center
1275 York Avenue . New York . N.Y. 10065