Case of the Month ...
Case History
A healthy 13 year-old boy was found by his mother to have a “pea-sized” lump on his right cheek, which increased substantially in size over the past year. The lesion did not responded to numerous antibiotic treatments. A fine needle aspiration (FNA) biopsy was performed and followed by a right parotidectomy.
Diagnosis & Discussion
click on image for larger version
Image Figs:
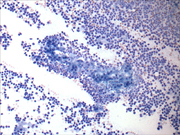
- Figure 1: FNA cytology, Papanicolaou stain, X40
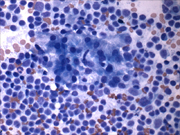
- Figure 2: FNA cytology, Diff-Quik stain, X200
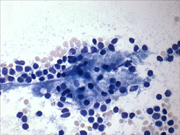
- Figure 3: FNA cytology, Papanicolaou stain, X200
- Figure 4: FNA cytology, Diff-Quik stain, X400
- Figure 5: FNA cytology, Diff-Quik stain, X400
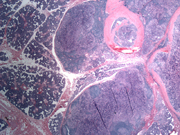
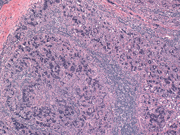
- Figure 6: Surgical resection, H&E stain, X 20
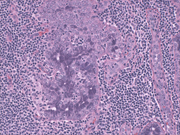
- Figure 7: Surgical resection, H&E stain, X 100
- Figure 8: Surgical resection, H&E stain, X 200
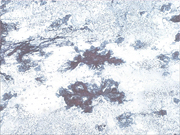
- Figure 9: Surgical resection, PAS stain, X 200
Questions:
- What is the diagnosis?
- Warthin's tumor
- Oncocytoma
- Mucoepidermoid carcinoma
- Acinic cell carcinoma
- In what salivary gland does this tumor occur most commonly?
- Parotid gland
- Sublingual gland
- Submandibular gland
- Minor salivary glands
- Which of the following statements is true regarding this tumor?
- It is always malignant
- The aspirates show dyscohesive clusters of epithelial cells with foamy, vacuolated or granular cytoplasm
- A significant lymphoid population is present in most cases
- Histologically, the tumor has a homogeneous growth pattern
- Which is the most common malignant salivary gland tumor in pediatric patients?
- Warthin's tumor
- Oncocytoma
- Mucoepidermoid carcinoma
- Acinic cell carcinoma
Discussion: Parotid gland neoplasms are quite rare in the pediatric population but when such a lesion is encountered, a higher percentage (40-50%) will be malignant when compared to the adult population (25-35%); therefore, parotid neoplasms in children must be approached with suspicion (1).
The mean age at which malignant parotid gland neoplasms occur in the pediatric population is 13.2 years (2). Acinic cell carcinoma (ACC) accounts for an appreciable number of pediatric parotid malignancies; in fact, it is the second most common malignant parotid tumor in this population followed by mucoepidermoid carcinoma (3). Nasse first described the lesion in a 1892 publication in which four cases of parotid adenomas were described (4). Due to the similarity of the tumor cells to normal salivary tissue, the lesions were initially regarded as benign. The benignity of the lesion was questioned in 1953 when Buxton et al. reported three cases of ACC with verified distant metastases (5).
Therefore, the lesion was previously termed “acinic cell tumor” to convey its somewhat unpredictable behavior. Currently, the lesion is characterized as “a malignant epithelial neoplasm in which, at least, some tumor cells demonstrate differentiation toward serous acinar cells” (6,7). It is considered an adenocarcinoma with low-grade malignant potential; therefore, the current terminology is acinic cell carcinoma. In the population at large, ACC is the fourth most common malignant salivary gland tumor (7-18% of malignant parotid neoplasms), occurs most commonly in the parotid gland, and has a mean age of 40-49 years at diagnosis but has been reported in ages 3 to 91 years (3,7,8).
The lesion typically presents as a slow growing, circumscribed, mobile mass which is tender in 33-50% of patients (6,7). An FNA of the lesion is characterized by a hypercellular specimen composed of dyscohesive sheets and clusters of cells with foamy, vacuolated cytoplasm with bland nuclei (6,9). Zymogen granules may be evident within the cytoplasm and a capillary meshwork with the loosely adherent cells may be appreciated on FNA (9).
Diagnosis of ACC on FNA relies almost entirely on recognition of acinar-type cytoplasmic differentiation. Histologically, the lesion is well circumscribed with sparse stroma. The cellular component displays acinar cells, intercalated ductal cells, and vacuolated cells. Zymogen granules may be present in variable amounts and are PAS positive and diastase resistant. Multiple histologic variants are observed including solid, microcystic, papillary-cystic, and follicular (7).
Ten to thirty-three percent of tumors may have a significant lymphoid background, as seen in this case presentation, making a possible diagnostic pitfall Warthin's tumor (6,9). Additionally, clear cell changes may occur which may lead one to consider metastatic renal cell carcinoma. The option for treatment is surgical excision. The risk of recurrence after surgical excision is 30 % and the risk of metastases and mortality are each 13% (7).
Unfortunately, attempts to predict patient outcome based on tumor histology have not been successful. Currently, the clinical stage at presentation is the most important predictor of prognosis (7).
Answers
- d
- a
- b
- c
REFERENCES
Ellies M, Laskawi R. Diseases of the salivary glands in infants and adolescents. Head Face Med 2010; 6:1.
Orvidas LJ, Kasperbauer JL, Lewis JE, Olsen KD, Lesnick TG. Pediatric parotid masses. Arch Otolaryngol Head Neck Surg 2000; 126:177-184.
Kim SA, Mathog RH. Acinic cell carcinoma of the parotid gland: a 15-year review limited to a single surgeon at a single institution. Ear Nose Throat J 2005; 84:597-602.
Fox NM Jr, ReMine WH, Woolner LB. Acinic cell carcinoma of the major salivary glands. Am J Surg 1963; 106:860-867.
Gustafsson H, Lindholm C, Carlsoo B. DNA cytophotometry of acinic cell carcinoma and its relation to prognosis. Acta Otolaryngol 1987; 104:370-376.
Luna MA. Salivary glands. In: Pilch BZ, Weinberg RW, Snyder A, et al., eds. Head and Neck Surgical Pathology . Philadelphia: Lippincott Williams & Wilkins; 2001, Chapter 8.
Gnepp DR, Henley JD, Simpson RHW, Everson J. In: Gnepp DR, ed. Diagnostic Surgical Pathology of the Head and Neck . 2 nd ed. Philadelphia: Saunders Elsevier; 2009, p476-481.
Goldman NC, Lee J, Tolley B. Acinic cell carcinoma of the parotid gland. Otolaryngology Head Neck Surg 2007; 137:828-829.
Nagel H, Laskawi R, Buter JJ, Schroder M, Chilla R, Droese M. Cytologic diagnosis of acinic-cell carcinoma of salivary glands. Diagn Cytopathol 1997; 16:402-412.
Contributed by Andrea Lynne Barbieri, MD and Guoping Cai, MD
Department of Pathology, Yale University School of Medicine