Case of the Month ...

Case History
A 46-year-old man presented with complaint of injection of the left sclera and proptosis. The MRI scan showed a 2.8 cm intraocular mass involving the left orbit and compressing the left lateral rectus muscle. Intraocular FNA biopsy was performed using a 25-gauge needle and followed surgical resection of the tumor.
Diagnosis & Discussion
click on image for larger version
Image Figs:
Figure 1: MRI image of the orbit
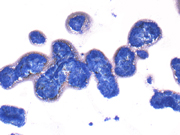
Figure 2: FNA cytology, Diff-Quik stain, X40
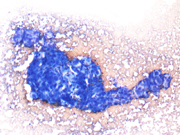
Figure 3: FNA cytology, Diff-Quik stain, X200
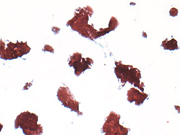
Figure 4: FNA cytology, Papanicolaou stain, X40
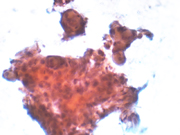
Figure 5: FNA cytology, Papanicolaou stain, X200
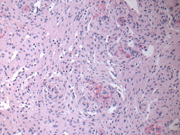
Figure 6: Surgical resection, H&E stain, X100
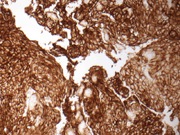
Figure 7: Surgical resection, EMA immunoperoxidase stain, X100
Questions:
What is the diagnosis?
Schwannoma
Solitary fibrous tumor
Meningioma
Metastatic carcinoma
From where is this tumor in the orbit most likely derived?
Direct extension of dura-based tumor
Primary tumor of optic nerve sheath
Direct invasion of soft tissue-raised tumor
Metastatic tumor
Which of the following statements is true regarding this tumor?
The aspirates are pauci-cellular
The aspirates show three dimensional cohesive clusters of epitheloid to spindle cells
The presence of whorls is diagnostic
Tumor cells are pleomorphic with frequent mitoses
Which are the immunophenotypic features of this tumor?
Discussion:
EMA-, Vimentin+, S-100+
EMA-, Vimentin-, S-100+
EMA+, Vimentin-, S-100+
EMA+, Vimentin+, S-100-
Meningioma is a neoplasm derived from meningothelial cells. The vast majority of meningiomas arise in intracranial or intraspinal locations as dura-based masses. Intracranial meningiomas may involve optic nerve by direct extension. However, primary optic nerve sheath meningiomas are uncommon, accounting for 2% of all orbital tumors and 1-2% of all meningiomas. 1 One early study shows that 72% of intraocular meningiomas arise from the dural sheath of the optic nerve, and the remaining 28% are primary extradural meningiomas. 2 Clinical presentations of this intraocular lesion may be unique to its anatomic location, including visual loss, strabismus and proptosis. Without intervention, loss of vision is just the matter of time. 3
The aspiration cytomorphologic features of meningiomas are well described in the literature. 4-8 The aspirates of typical meningiomas are often cellular and consist of cohesive three-dimensional sheets or clusters of epitheloid to spindle cells, focally forming whorls in which cells are arranged in a onion-like fashion. The presence of whorls is a characteristic finding in meningiomas, but whorls can also be found in other entities such as squamous cell carcinoma. The whorls of meningiomas do not show any evidence of keratinization. Cytologically, the tumor cells are bland, relatively uniform, and have modest to copious bipolar cytoplasm and oval nuclei with fine chromatin and small nucleoli. Intranuclear inclusions are occasionally seen. Psammoma bodies may or may not be present. Histologic variants of meningiomas can display a wide range of cytomorphologic characteristics, which may impose diagnostic challenge. Meningiomas with clear cell, plasmacytoid cell or anaplastic features have also been described. 9-11
Differential diagnosis may include both non-neoplastic and neoplastic entities in the intraocular location. Inflammatory pseudotumors such as sarcodiosis, Rosai-Dorfman disease, and plasma cell granuloma could present as a meningioma-like mass. Schwannoma, solitary fibrous tumor, and hemangiopericytoma are the neoplastic lesions that should be differentiated from meningiomas. Characteristic cytomorphologic features of meningioma would be helpful render a correct diagnosis. In difficult cases, immunohistochemical studies should be performed. 12 The vast majority of meningiomas stain positive for EMA. Vimentin positivity is found in all meningiomas. There are variable stains for S-100. In addition, immunoreactivity for progesterone receptor is seen in most benign meningiomas.
Answers
- c
- a
- b
- d
REFERENCES
Eddleman CS, Liu JK. Optic nerve sheath meningioma: current diagnosis and treatment. Neurosurg Focus. 2007; 23(5): E4.
Fortuna A, Nicole S, Palma L, Di Lorenzo N. Primary intraorbital meningiomas. Riv Neurol. 1978; 48(3): 251-270.
Schick U, Jung C, Hassler WE. Primary optic nerve sheath meningiomas: a follow-up study. Cen Eur Neurosurg. 2010; 71(3): 126-133.
Silverman JF. Cytopathology of fine-needle aspiration biopsy of the brain and spinal cord. Diagn Cytopathol. 1986; 2(4): 312-319.
Rorat E, Yang W, DeLaTorre R. Fine needle aspiration cytology of parapharyngeal meningioma. Acta Cytol. 1991; 35(5): 497-500.
Baisden BL, Hamper UM, Ali SZ. Metastatic meningioma in fine-needle aspiration (FNA) of the lung: cytomorphologic finding. Diagn Cytopathol. 1999; 20(5): 291-294.
Mehrotra R, Kumar S, Singh K, Tandon MP, Singh M. Fine-needle aspiration biopsy of orbital meningioma. Diagnostic Cytopathology. 1999; 21(6): 402-404.
Amoli FA, Mehrabani PM, Tari AS. Aggressive orbital optic nerve meningioma with benign microscopic features: a case report. Orbit. 2007; 26(4): 271-274.
Imlay SP, Snider TE, Raab SS. Clear-cell meningioma: diagnosis by fine-needle aspiration biopsy. Diagn Cytopathol. 1998; 18(2): 131-136.
Nicolas MM, Kaakaji R, Russell EJ, De Frias DV, Nayar R. Extradural spinal meningioma as a source of plasmacytoid cells. A case report. Acta Cytol. 2007; 51(1): 68-72.
Ahuja A, Iyer VK, Gupta R, Suri V, Mathur SR, Arora R. Fine needle aspiration cytology of anaplastic meningioma. Cytopathology. 2010. DOI:10.1111/j.1365-2303.2010.00810.x.
Perry A, Louis DN, Scheithauer BW, Budka H, von Deimling A. Meningiomas. In: Louis DN, Ohgaki H, Wiestler OD, Cavenee WK (eds). WHO Classification of Tumours of the Central Nervous System. 4 th ed. Lyon: International Agency for Research on Cancer. 2007, p164-172.
Case contributed by
Yue Wu, MD, PhD and Guoping Cai, MD
Department of Pathology
Yale University School of Medicine