Case of the Month ...
Case History
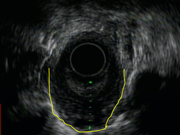
A 52-year-old woman presented with worsening dysphagia and inability to tolerate solids. She first noted the onset of mild symptoms 1-2 years ago. Four months ago, she felt that her symptoms were getting worse to the point that she modified her diet to mainly soft foods. About 2-3 weeks prior to presentation, she began experiencing dysphagia with both solids and liquids and noted a 50 lb unintentional weight loss over the last month. An EGD/EUS showed an esophageal mass measuring 1.5 cm in the middle third of the esophagus, with loss of wall layer pattern. The overlying mucosa appeared normal. Endoscopic ultrasound-guided FNA of the mass was performed using a 22G EUSN3 needle.
Diagnosis & Discussion
click on image for larger version
Image Figs:
- Figure 1: Endoscopic Ultrasound (EUS)
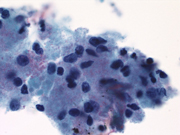
- Figure 2: FNA cytology, Diff-Quik stain, X400
- Figure 3: FNA cytology, ThinPrep, Papanicolaou stain, X1000
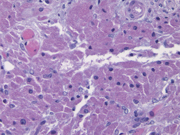
- Figure 4: FNA cytology, cell block, H&E stain, X400
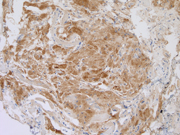
- Figure 5: FNA cytology, cell block, CD68 immunoperoxidase stain, X200
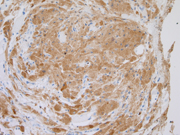
- Figure 6: FNA cytology, cell block, S100, immunoperoxidase stain, X200
Questions:
- What is the diagnosis?
- Leiomyoma
- Adenocarcinoma
- Granular cell tumor
- Hamartoma
- The cytoplasm of the cells most likely contain abundant:
- Mitochondria
- Hydrolytic enzyme-containing lysosomes
- Smooth muscle actin
- Endoplasmic reticulum
- Most patients with this lesion present with:
- Unrelated gastrointestinal symptoms
- Dysphagia
- Anemia
- Epigastric pain
- Which of the following is true regarding this lesion?
- There is an association with dysplasia of the overlying mucosa
- Pseudoepitheliomatous hyperplasia can be seen in the overlying epithelium
- Malignant transformation is common
- Surgical excision for all lesions is recommended
Discussion:
Granular cell tumors (GCTs) are relatively uncommon neoplasms that can be found in many locations including the oral cavity, orbit, skin, skeletal muscle, gastrointestinal tract, breast, external genitals, respiratory tract, biliary system, and peripheral and cranial nerves. Only about 5-11% of all GCTs arise in the gastrointestinal tract and of these, one-third occur in the esophagus. Esophageal GCTs are most commonly observed in the fifth decade of life with a female predilection. The majority of patients with GCTs of the esophagus do not report any symptoms attributable to the tumor and the lesion is discovered during the course of investigation for unrelated gastrointestinal issues. In patients who present with symptoms related to the GCT, the most commonly reported symptom is dysphagia.
Although the majority of cases of GCT are diagnosed by core needle biopsy, diagnosis by image-guided FNA has been reported. On Papanicolaou-stained preparations, tumor cells are arranged singly or in fragments with ill-defined cell margins, abundant basophilic granular cytoplasm, and bland-appearing round or spindle-shaped nuclei. Granules within the cell cytoplasm stain positive with Periodic Acid-Schiff as well as S-100 and CD68 immunostaining. The granular cytoplasm is thought to contain numerous hydrolytic enzyme-containing lysosomes. GCTs are characterized histologically by large cells with abundant granular cytoplasm, bland nuclei, and indistinct nucleoli. Signs of malignancy include an infiltrative growth pattern, size larger than 4 cm, evidence of rapid growth, recurrence after primary resection, nuclear pleomorphism, tumor cell necrosis, spindling, and 2 or more mitoses per 10 high power fields. GCTs of the skin, larynx, and esophagus are known to induce pseudoepitheliomatous hyperplasia in the overlying epithelium, a feature that may simulate squamous cell carcinoma.
The vast majority of GCTs of the esophagus have an indolent clinical course. The optimum treatment for these lesions is dependent upon the size of the tumor and the presence or absence of symptoms. A conservative approach with regular endoscopic follow-up is recommended for tumors <10 mm in diameter. Tumors >20 mm, those causing symptoms, or those clinically concerning for malignancy should be surgically excised. Endomucosal resection has been shown to effectively and safely remove tumors that meet specific criteria (<20 mm without attachment to the muscle layer).
Answers
- C
- B
- A
- B
REFERENCES
• Huang AT, Dominguez LM, Powers CN, Reiter ER. Granular Cell Tumor of the Cervical Esophagus: Case Report and Literature Review of an Unusual Cause of Dysphagia. Head Neck Pathol. 2012 Nov 11.
• Prematilleke IV, Piris J, Shah KA. Fine needle aspiration cytology of a granular cell tumour of the oesophagus. Cytopathology. 2004 Apr;15(2):120-1.
• Szumilo J, Dabrowski A, Skomra D, Chibowski D. Coexistence of esophageal granular cell tumor and squamous cell carcinoma: a case report. Dis Esophagus. 2002;15(1):88-92.
• Narra SL, Tombazzi C, Datta V, Ismail MK. Granular cell tumor of the esophagus: report of five cases and review of the literature. Am J Med Sci. 2008 May;335(5):338-41.
• Nakajima M, Kato H, Muroi H, Sugawara A, Tsumuraya M, Otsuka K, Domeki Y, Onodera S, Sasaki K, Tsubaki M, Sohda M, Miyazaki T, Kuwano H. Esophageal granular cell tumor successfully resected by endoscopic submucosal dissection. Esophagus. 2011 Sep;8(3):203-207. Epub 2011 Jul 14.
• Zhong N, Katzka DA, Smyrk TC, Wang KK, Topazian M. Endoscopic diagnosis and resection of esophageal granular cell tumors. Dis Esophagus. 2011 Nov;24(8):538-43.
• Mohammad S, Naiditch JA, Jaffar R, Rothstein D, Bass LM. Granular cell tumor of the esophagus in an adolescent girl. J Pediatr Gastroenterol Nutr. 2012 Jun;54(6):715.
Contributed by
Joseph Hatem, MD
Gordon Yu, MD
Hospital of University of Pennsylvania,
Department of Pathology and Laboratory Medicine