Case of the Month ...
Clinical History:
A 50 year-old female patient was found to have a thyroid nodule on a routine physical examination. She has no complaints of hoarseness, swallowing difficulty, or other symptoms. Ultrasound scan revealed a 3.5-cm solid nodule with increased vascularity in the right lobe of the thyroid and multiple enlarged abnormal-appearing lymph nodes with calcifications in the right neck. Ultrasound-guided fine needle aspiration (FNA) of the right thyroid nodule was performed.
Diagnosis & Discussion
click on image for larger version
Image Figs:
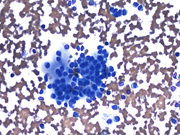
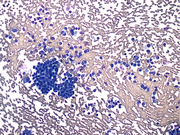
Figure 1: FNA cytology, Diff-Quik stain, X200
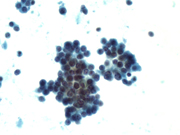
Figure 2: FNA cytology, Diff-Quik stain, X400
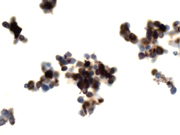
Figure 3: FNA cytology, Papanicolaou stain, X400
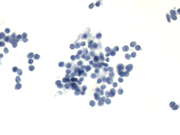
Figure 4: FNA cytology, Papanicolaou stain, X400
Figure 5: FNA cytology, calcitonin immunoperoxidase stain, X400
Figure 6: FNA cytology, thyroglobulin immunoperoxidase stain, X400
Questions:
What is the diagnosis?
- Poorly differentiated thyroid carcinoma
- Primary small cell carcinoma of the thyroid
- Medullary thyroid carcinoma, small cell variant
- Metastatic small cell carcinoma
- Which are the typical cytomorphologic features of this tumor?
- Pleomorphic atypical cells, mitosis and necrosis
- Monomorphic small cells with salt and pepper chromatin pattern and scant cytoplasm
- Intermediate sized cells with nuclear molding, crush artifact, apoptosis, mitosis and necrosis
- Plasmacytoid and spindle cells with finely granular chromatin
- Which are the typical immunophenotypic features of this tumor?
- Thyroglobulin+, TTF-1+, CEA-, calcitonin-
- TTF-1+, Synaptophysin+, chromogranin+, CEA-, calcitonin-
- TTF-1-, Thyroglobulin-, CEA-, LCA+
- Thyroglobulin-, CEA+, calcitonin+
- What gene mutation or variation can occur in multiple endocrine neoplasia type (MEN) 2a and MEN 2b ?
- RET
- ALK
- BRAF
- RAS
Discussion:
Medullary thyroid carcinoma (MTC) is a malignant neoplasm derived from parafollicular C-cells. MTC comprises approximately 3-10% of thyroid carcinomas and can occur in sporadic (75-80% of cases) or heritable forms (multiple endocrine neoplasia [MEN] 2a, MEN 2b and familial medullary thyroid carcinoma [FMTC]). Patients with sporadic MTC and FMTC present at the age of 44-50 years and usually have a solitary thyroid nodule. These patients can have paraneoplastic syndromes such as diarrhea and Cushing's syndrome. The patients with MEN 2a and MEN 2b are younger and often have bilateral, multiple tumor nodules that are associated C-cell hyperplasia. The hereditary forms of MTC are caused by germline mutations of the RET proto-oncogene. MTC is an indolent but aggressive tumor that spreads via hematogenous and lymphatic routes. Up to 50% of patients have cervical nodal metastasis at the presentation.
The classic cytomorphologic features of MTC include single and discohesive clusters of intermediate sized to large cells with plasmacytoid, polygonal, or spindle shape and finely granular chromatin. Amyloid is often present as dense amorphous material. MTC is usually immunoreactive with calcitonin, CEA, chromogranin, synaptophysin. TTF-1 immunostain is variable. However, MTC has a variety of morphologic variants, including papillary, glandular, giant cell, spindle cell, small cell, neuroblastoma-like, paraganglioma-like, oncocytic, clear cell, pseudoangiosarcoma, squamous cell, melanin-producing and amphicrine variants. This morphologic heterogeneity may impose a diagnostic challenge.
Small cell variant of MTC (SCV-MTC) is a well-recognized form of MTC and has less favorable outcome than the typical MTC. SCV-MTC is characterized cytologically by single and dyscohesive clusters of small round to oval cells with scant cytoplasm and finely granular (“salt and pepper”) chromatin. Amyloid may or may be present as dense, amorphous colloid-like material. The differential diagnosis of SCV-MTC includes poorly differentiated thyroid carcinoma, metastatic small cell carcinoma, primary small cell carcinoma of the thyroid, and non-Hodgkin lymphoma. Immunostaining is crucial in rendering diagnosis of SCV-MTC. SCV-MTC is immunoreactive with calcitonin, CEA, chromogranin and synaptophysin; while negative for thyroglobulin and LCA. Rarely SCV-MTC may show focal or no reactivity for calcitonin.
Poorly differentiated thyroid carcinoma is a thyroid carcinoma of follicular cell origin, characterized by its insular, solid or trabecular growth patterns with mitosis, apoptosis and necrosis. The neoplastic cells have high nuclear to cytoplasmic ratios with variable nuclear atypia but lack neuroendocrine chromatin features. Cell groups with endothelial wrapping or fibrotic stroma, the reminiscent of insular growth pattern, can sometimes be seen in the fine needle aspirats. The tumor cells are positive for thyroglobulin and negative for calcitonin and CEA.
Metastatic small cell carcinoma is featured with isolated or loosely cohesive clusters of small to intermediate cells with scant cytoplasm, nuclear molding and finely granular chromatin. Smearing crush artifact, apoptosis, and necrosis are often present. Primary sites may include lung and extrapulmonary sites. Metastatic small cell carcinoma is positive for cytokeratin, TTF-1, chromogranin, synaptophysin, CD56; while negative for calcitonin and CEA.
Primary small cell carcinoma of the thyroid is a rare entity, which shares similar cytomorphologic features with metastatic small cell carcinoma. The tumor in two reported cases is positive for chromogranin and synaptophysin, while negative for thyroglobulin and calcitonin.
Non-Hodgkin Lymphomas can secondarily involve the thyroid or arise de nova in the thyroid. The majority of primary thyroid lymphomas are B-cell lymphomas, including diffuse large B-cell lymphoma (DLBCL) and extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue (MALToma). Lymphoma is usually composed of dispersed single cells with numerous lymphoglandular bodies in the background. The tumor cells of MALToma are small, relatively uniform, and have vesicular; while the cells in DLBCL are large, pleomorphic, and have coarse chromatin and prominent nucleoli. Flow cytometry and immunocytochemistry are most helpful in the diagnosis of non-Hodgkin B-cell lymphomas.
In summary, the cytomorphologic features of SCV-MTC include single and dyscohesive clusters of small tumor cells with scant cytoplasm and finely granular (salt and pepper) chromatin with presence or absence of amyloid. The tumor is positive for calcitonin and CEA, and negative for thyroglobulin. Theses cytomorphologic and immunophenotypic features are helpful in the differential diagnosis of SCV-MTC with the typical MTC and other tumors with small cell morphology.Answer Key:
- c
- b
- d
- a
REFERENCES
Matias-Guiu X, DeLellis R, Moley JF et al. Medullary thyroid carcinoma. In: DeLellis RA, Lloyd RV, Heitz PU, eds. World Health Organization Classification of Tumors Pathology and Genetics of Endocrine Organs. Lyon: IARC Press, 2004, p86-91.
Rosai J, Carcangiu ML, DeLellis RA. Medullary carcinoma. In: Rosai J, Sobin LH, eds. Atlas of Tumor Pathology: Tumors of the Thyroid Gland. Third Series. Washington: Armed Forces Institute of Pathology, 1992, p207-245.
Yerly S, Triponez F, Meyer P, et al. Medullary thyroid carcinoma, small cell variant as a diagnostic challenge on fine needle aspiration a case report. Acta Cytol 2010; 54(suppl):911-917.
Bongiovanni M, Bloom L, Krane JF, et al. Cytomorphologic features of poorly differentiated thyroid carcioma: A multi-institutional analysis of 40 cases. Cancer Cytopathol 2009; 117:185-194.
Layfield LJ, Gopez EV. Insular carcinoma of the thyroid: Report of a case with intact insulae and microfollicular structures. Diagn Cytopathol 2000; 23:409-413.
Matias-Guiu X, LaGUette J, Puras-Gil AM, Rosai J. Metastatic neuroendocrine tumors to the thyroid gland mimicking medullary carcinoma: A pathologic and immunohistochemical study of six cases. Am J Surg Pathol 1997; 21:754-762.
Eusebi V, Damiani S, Riva C, et al. Calcitonin free oat-cell carcinoma of the thyroid gland. Virchows Arch A Pathol Anat Histopathol 1990; 417:267-271.
Cha C, Chen H, Westra WH, Udelsman R. Primary thyroid lymphoma: can the diagnosis be made solely by fine-needle aspiration? Ann Surg Oncol 2002; 9:298-302.
Gupta N, Nijhawan R, Srinivasan R, et al. Fine needle aspiration cytology of primary thyroid lymphoma: a report of ten cases. Cytojournal 2005; 2:21.
Contributed by:
Xiu Sun, M.D., Ph.D.
Guoping Cai, M.D.,
Department of Pathology
Yale University School of Medicine