Case of the Month ...
Clinical History:
A 52-year-old man presented with multiple intrapelvic masses on CT scan. CT-guided fine needle aspiration and core biopsies of one of the pelvic masses were undertaken. He had a history of an intrabdominal neoplasm resected two years ago.
Diagnosis & Discussion
click on image for larger version
Image Figs:
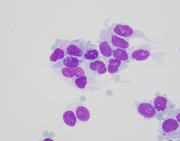
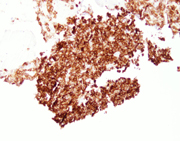
Figure 1: FNA cytology, Diff-Quik, x40.
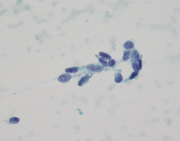
Figure 2: FNA cytology, Diff-Quik, x400.
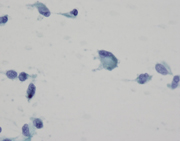
Figure 3: FNA cytology, PAP, x400.
Figure 4: FNA cytology, PAP, x400.
Figure 5: FNA cytology, Cell block, H&E, x100
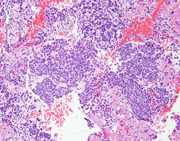
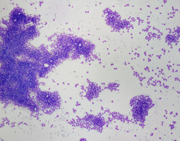
Figure 6: Concurrent core needle biopsy, CD117 (c-Kit) immunostaining, x100
Questions:
Which of the following is an appropriate differential diagnosis of this lesion depicted in the pictures?
- Schwannoma
- Leimyosarcoma
- Gastrointestinal stromal tumor (GIST)
- Fibromatosis
- All of the above
- Which panel of immunostains is commonly used to confirm the diagnosis?
- CD34 and SMA
- CD99 and SMA
- CD117 and CD34
- CD117 and CD99
- Which of the immune markers is sensitive and specific for diagnosing KIT-negative GIST?
- PDGFRA
- beta-catenin
- DOG1
- CD99
- Which of the parameters listed below are used to evaluate the biologic behavior of GISTs (choose the best answer)?
- Necrosis and mitotic activity
- T umor size and mitotic activity
- Infiltrating border and necrosis
- Cellular pleomorphism and percentage of spindle and epitheliod component
- Which of the organs/anatomic locations listed below are the most common sites that GISTs tend to metastasize to?
- Lung and lymph node
- Lung and bone
- Pelvic cavity and lymph node
- Pelvic cavity and liver
- Soft tissue and skin
Discussion:
The smears and cell block sections are highly cellular, and show numerous isolated, clusters and solid nests of epithelioid and spindled neoplastic cells with large, convoluted nuclei, visible nucleoli and scant to moderate cytoplasm. Occasional binucleation, intranuclear inclusions and perinuclear vacuoles are evident. Immunohistochemical stains on the concurrent core biopsy show that the neoplastic cells are diffusely positive for CD117(c-Kit), but negative for CD34. Proliferation index by MIB1 labeling is approximately 10%. Mutational analysis reveals a mutation in KIT exon 11, while no activating mutations in the PDGFRA gene detected. These findings, despite the absence of CD34 immunoreactivity, are consistent with pelvic GIST, in this case, being recurrent.
GISTs are of interstitial Cajal origin, and are the most common mesenchymal neoplasms of the GI (gastrointestinal) tract. These tumors most commonly arise from the stomach (50%), followed by the small intestine (25%), the colon and rectum (10%), and the esophagus (5%). Approximately 10% of GISTs occur outside the GI tract, primarily in the mesentery, omentum and retroperitoneum, and have been referred as EGIST (extragastrointestinal stromal tumors). This patient had undergone surgery for a high risk pelvic GastroIntestinal Stromal Tumor (GIST) two years ago, and presented for follow up with recurrent pelvic nodules. He had received adjuvant Imatinib (Gleevec) therapy shortly after his surgery, but the medication was later discontinued at patient's request.
Microscopically, GISTs may show spindled (70%), epithelioid (20%), or mixed (10%) cell morphologies. The spindled cell type may exhibit interlacing, short fascicles or a short, storiform growth pattern. The cells are usually monomorphic, with rounded to elongated nuclei show ing fine open chromatin, inconspicuous nucleoli, and abundant eosinophilic fibrillary cytoplasm with indistinct cell borders. The epithelioid cell type may consist of cohesive epitheliod cells with a syncytial appearance or dyscohesive cells with a sharp cell borders. Stromal collagen deposition is generally minimal. The epithelioid cells are polygonal with round nuclei displaying small nucleoli and moderate amounts of amphophilic cytoplasm. Other cytologic features often seen in GISTs are cytoplasmic vacuoles and bi- and multi-nucleation. The vacuoles are perinuclear, sometimes encroach on the nucleus or coalesce, creating signet ring-like appearance.
Approximately 20-25% of gastric and 40-50% of small intestinal GISTs are clinically malignant. The recognized prognostic factors of GISTs include tumor size, mitotic index and tumor location. Small intestinal GISTs are more likely to be malignant compared to gastric GISTs of similar size and mitotic activity. Although less data is available for EGISTs, it has been suggested that they should be assessed as small intestinal GISTs. The most common metastatic sites are abdominal cavity and liver, while other sites are rare. No lymph nodes or lung metastases have been reported so far. All patients with GISTs should be followed up for long time because of well-known late relapse.
By immunohistochemistry, more than 95% of GISTs are c-KIT (CD117) positive. The staining is usually strong and diffuse, mostly cytoplasmic, or dot-like (Golgi pattern), or membranous. However, positive immunoreactivity to c- KIT is not specific for GIST. Other neoplasms including malignant melanoma, synovial sarcoma, mesenteric fibromatosis (desmoid tumors), schwannoma, mastocytosis, seminoma, pulmonary small cell carcinoma, angiosarcoma and granulocytic sarcoma have been reported to be immunohistochemically positive for c-KIT. Strict staining control and interpretation, and an extended panel of markers can facilitate determination of an accurate diagnosis. Other markers can be positive in GIST, and often included in the panel, including CD34 (60-70%), smooth muscle actin (30-40%), h-Caldesmon (85%), S100 (5%), and desmin (1-2%). DOG1, a recently discovered immunostain marker for GISTs, has high sensitivity (70-100%) and specificity for GISTs. DOG1 is especially useful in diagnosing KIT-negative GISTs.
Most GISTs are sporadic. Less than 5% of GISTs are associated with tumor syndromes including neurofibromatosis type 1, Carney triad, and familial GIST syndrome. The majority of the GISTs (85-90%) have an underlying driven mutation in the KIT gene. Some of the remainder contains mutations in PGFRA (platelet derived growth factor receptor-alpha) gene. Approximately 5-10% of GISTs are negative for both KIT and PDGFRA mutations, suggesting a different molecular mechanism. GISTs with PDGFRA often have epithelioid morphology and generally occur in the stomach. Detection of the mutation type and site has become important in considering therapy. Gleevec, which is a tyrosine kinase inhibitor, exhibits different therapeutic effects on GISTs with different mutations. For example, KIT mutations on exon 11 predict a great response, while exon 13 or exon 17 mutations are relatively resistant and exon 9 mutations respond to a higher dose of Imatinib.
Answers:
1. e
2. c
3. c
4. b
5. dCase contributed by
Huimiao (Mia) Jiang, MD, PhD and Xiao-Jun Wei, MD
NYU School of Medicine
Department of Pathology
New York, NY