Case of the Month ...
A 67-year-old male with a recently diagnosed and resected clear cell renal cell carcinoma presented with a two-month history of abdominal pain and weight loss. Imaging studies revealed a 1.5 cm pancreatic head mass, suspicious for metastasis. The patient underwent a fine-needle aspiration (FNA) of the pancreatic mass.
Authors
- Lagnajita Datta
Diagnosis & Discussion
click on image for larger version
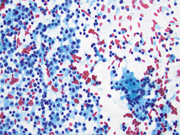
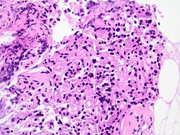
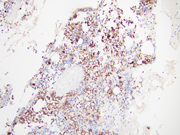
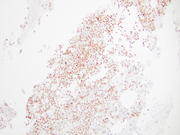
Figure 3 Figure 4 Figure 5 Figure 6 Images 1-6:
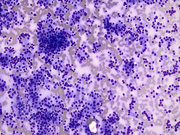
- Figure 1: Diff-Quik Stain, 200x
- Figure 2: Papanicolau Stain, 400x
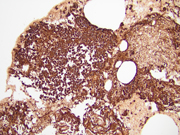
- Figure 3: Cell block, Hematoxylin and Eosin (H&E) stain, 400x
- Figure 4: Cell block, AE1/AE3, 200x
- Figure 5: Cell block, PAX8, 200x
- Figure 6: Cell block, Chromogranin, 200x
Additionally, neoplastic cells were positive for TTF-1 (rare, scattered) and negative for CK7, Napsin-A and p40 (images not shown).
Questions:
- What is the diagnosis?
- Pancreatic adenocarcinoma
- Pancreatic neuroendocrine tumor, well differentiated
- Metastatic renal cell carcinoma (RCC)
- Acinar cell carcinoma
- Which of the following statements is true for pancreatic neuroendocrine tumors?
- Are classified based on mitotic count and proliferative index (Ki-67).
- Are positive for neuroendocrine immunohistochemical markers like INSM1, synaptophysin and chromogranin and can be positive for PAX8 (polyclonal).
- Can be associated with familial syndromes like von Hippel Lindau (VHL) and MEN syndromes
- All of the above.
- None of the above.
Answers:
Question 1: Correct answer is B
Differentiation between metastatic clear cell renal cell carcinoma (RCC) and pancreatic neuroendocrine tumor (PanNET) on cytopathological and immunohistochemical evaluation can be challenging, as both tumors can have overlapping morphological and immunohistochemical features. Clear cell RCC metastases to the pancreas can have similar cytomorphological features to PanNETs, with small uniform cells arranged in nests and trabeculae. However, RCC cells typically have more abundant cytoplasm with a clear appearance, and may have intracytoplasmic vacuoles. In contrast, PanNET cells have scant cytoplasm, plasmacytoid morphology and display a "salt and pepper" chromatin pattern. Clear cell RCC cells express RCC marker PAX8 and CAIX. PanNETs, on the other hand, express neuroendocrine markers such as INSM1, synaptophysin, chromogranin A, and CD56, which are typically negative in clear cell RCC. An important pitfall to remember is that clear cell change and PAX8 positivity can be seen in PanNETs, making the differential diagnosis challenging. In fact, PAX8 (polyclonal) can be used to distinguish PanNETs from ileal and pulmonary well-differentiated neuroendocrine tumors, especially in cases with metastasis. Other differentials include pancreatic adenocarcinoma, solid pseudopapillary neoplasm (SPN) and acinar cell carcinoma. However, the cytomorphology along with the presence of immunohistochemical neuroendocrine markers such as INSM1 and chromogranin A make the diagnosis of a neuroendocrine tumor more likely.Question 2: Correct answer is D
According to the WHO classification, pancreatic neuroendocrine neoplasms (PanNENs) are malignant and are classified as well-differentiated NENs, called neuroendocrine tumours (PanNETs), and poorly differentiated NENs, designated neuroendocrine carcinomas (PanNECs), which can be either small cell or large cell type. All PanNENs show positivity for neuroendocrine markers such as INSM1, synaptophysin and chromogranin. PanNETs can be further classified based on their mitotic activity and proliferative index (Ki-67) into three categories: well-differentiated tumors (grade 1 and 2), poorly differentiated tumors (grade 3), and mixed exocrine-neuroendocrine tumors.Cytology plays a crucial role in the diagnosis of PanNETs, as it allows for the evaluation of the tumor's cellular characteristics and can aid in the differentiation between PanNETs and other pancreatic tumors. On cytological evaluation, cellular smears with small uniform cells that have round nuclei and scant cytoplasm, plasmacytoid morphology and uniform round-to-oval nuclei with coarse granular chromatin and inconspicuous nucleoli are noted. The cells may form nests or trabeculae and are often arranged in a loosely cohesive pattern as well as single cells. Mitotic figures and necrosis are usually not identified. Grading in cytological specimens can underestimate the true grade because of limited material.
PanNETs can be associated with hereditary syndromes, such as multiple endocrine neoplasia type 1, von Hippel Lindau syndrome (VHL), tuberous sclerosis, type 1 neurofibromatosis, glucagon cell hyperplasia and neoplasm syndrome (Mahvash disease), familial insulinomatosis, Lynch syndrome, and familial atypical multiple mole melanoma (FAMMM) syndrome. Important point to note is that metastasis from renal cell carcinoma may mimic a clear cell variant of PanNET, particularly in the setting of VHL.References:
- Hoang MP, Hruban RH, Albores-Saavedra J. Clear cell endocrine pancreatic tumor mimicking renal cell carcinoma: a distinctive neoplasm of von Hippel-Lindau disease. Am J Surg Pathol. 2001 May;25(5):602-9. doi: 10.1097/00000478-200105000-00006. PMID: 11342771.
- Bellizzi AM. Immunohistochemistry in the diagnosis and classification of neuroendocrine neoplasms: what can brown do for you? Hum Pathol. 2020 Feb;96:8-33. doi: 10.1016/j.humpath.2019.12.002. Epub 2019 Dec 17. PMID: 31857137; PMCID: PMC7177196.
- Sangoi AR, Ohgami RS, Pai RK, Beck AH, McKenney JK, Pai RK. PAX8 expression reliably distinguishes pancreatic well-differentiated neuroendocrine tumors from ileal and pulmonary well-differentiated neuroendocrine tumors and pancreatic acinar cell carcinoma. Mod Pathol. 2011 Mar;24(3):412-24. doi: 10.1038/modpathol.2010.176. Epub 2010 Oct 1. PMID: 20890270.