Case of the Month ...
A 44-year-old female presented with cough and shortness of breath. Imaging revealed large bilateral pleural effusion and a 17 x 12 cm solid and cystic pelvic mass. Cytospins and cell block of the pleural fluid were prepared (Figures 1-5).
Authors
- Yan Gao, MD, Y. Helen Zhang, MD. Department of Pathology and Laboratory Medicine, The University of Texas Health Science Center at Houston
Diagnosis & Discussion
click on image for larger version
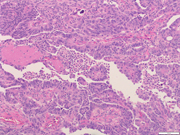
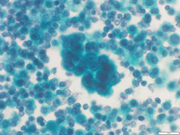
Figure 3 Figure 4 Figure 5 Figure 6 Images 1-6:
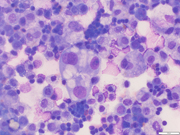
- Figure 1: Cytospin, Papanicolaou stain, 400x
- Figure 2: Cytospin, Diff-Quik stain, 400x
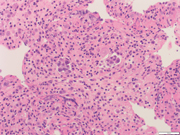
- Figure 3: Cell block, Hematoxylin and Eosin (H&E) stain 200x
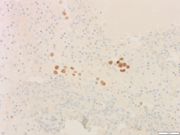
- Figure 4: Cell block, PAX8 immunohistochemical stain 200x
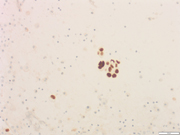
- Figure 5: Cell block, P53 immunohistochemical stain 200x
- Figure 6: Histology, of resection, Hematoxylin and Eosin (H&E) stain 100x
Questions:
- Based on the images, what is the most likely diagnosis and what immunohistochemical markers will be positive?
- Adenocarcinoma, gastrointestinal tract origin; MOC-31, CDX2
- Metastatic lung adenocarcinoma; MOC-31, TTF-1
- Adenocarcinoma, Mullerian origin; MOC-31, PAX-8
- Metastatic breast carcinoma; MOC-31, GATA-3
- Which of the following is true of patients who carry BRCA1 mutation?
- Females with a pathogenic BRCA1 variant have approximately a 65%-79% lifetime risk of breast cancer.
- Targeting DNA damage repair with poly (ADP-ribose) polymerase (PARP) inhibitors as a maintenance therapy for high-grade serous carcinoma significantly improves progression-free survival for BRCA1 carriers.
- Patients with BRCA1 germline mutations have significantly better prognosis.
- All of the above
Answers:
Question 1: Correct answer is CThe cytospins (Figure 1, 2) and cell block (Figure 3) show clusters of malignant epithelial cells exhibiting marked nuclear atypia, high nuclear-to-cytoplasmic ratio and cytoplasmic vacuoles. Some of the cells are arranged in a glandular or papillary pattern. Immunostains performed on the cell block sections show that the tumor cells are positive for MOC-31, CK7, PAX-8 (Figure 4), and p53 (Figure 5, mutation-type labelling), while negative for CK20, TTF-1, and CDX2. These findings are compatible with a metastatic adenocarcinoma of Mullerian origin.
Two months later, the patient underwent hysterectomy, bilateral salpingo-oophorectomy, and omentectomy. The tumor (Figure 6) demonstrates a mixed papillary and solid growth pattern. The tumor cells were positive for WT1, p53 (diffuse and strong) and p16 (diffuse and strong). The overall morphology and immunoprofile are characteristic of a high-grade serous carcinoma. Since this patient was diagnosed with ovarian cancer at a relatively young age, genetic testing was performed, and a pathogenic/deleterious mutation was detected in the BRCA1 gene.Question 2: Correct answer is D
High-grade serous carcinomas typically originate from tubal-type epithelium, primarily in the fallopian tube fimbria. Approximately 15% of cases can be attributed to germline mutations in BRCA1 or BRCA2. BRCA1 is a critical tumor suppressor gene involved in DNA repair processes, particularly in maintaining genomic stability. Pathogenic variants in BRCA1 disrupt its normal functioning, leading to an increased susceptibility to cancer development. Females carrying a pathogenic BRCA1 variant face a significantly elevated lifetime risk of approximately 65%-79% for developing breast cancer, underscoring the importance of identifying and assessing BRCA1 mutations in affected individuals. In addition, the lifetime risk for ovarian, fallopian tube, or peritoneal cancer in affected individuals with BRCA1 mutations ranges from 16% to 59%. The identification of BRCA1 mutations is crucial in assessing the genetic predisposition and potential risks associated with high-grade serous carcinomas. By understanding the impact of BRCA1 on cancer development, it becomes possible to implement appropriate screening and preventive measures for at-risk individuals. Targeting DNA damage repair with poly (ADP-ribose) polymerase (PARP) inhibitors as a maintenance therapy for high-grade serous carcinoma can significantly improve progression-free survival for both BRCA1/2 carriers.
REFERENCES
- WHO Classification of Tumours, 5th ed, Female Genital Tumours Lyon (France): International Agency for Research on Cancer; page 45-47, 2020.
- Karoline B Kuchenbaecker, Håkan Olsson, etc. Risks of Breast, Ovarian, and Contralateral Breast Cancer for BRCA1 and BRCA2 Mutation Carriers. JAMA, 2017 Jun 20;317(23):2402-2416. doi: 10.1001/jama.2017.7112.
- Antoniou A, Pharoah P.D.P, etc. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case Series unselected for family history: a combined analysis of 22 studies. Meta-Analysis: Am J Hum Genet, 72(5), 1117-1130. doi: 10.1086/375033.