Case of the Month ...
A 53-year-old female presented with intermittent postmenopausal bleeding. An ultrasound showed multiple submucosal, subserosal and cervical fibroids. A Pap test was performed, and the concurrent high-risk human papillomavirus test (HR-HPV) was negative. Cervical myomectomy was performed.
Authors
- Niyati Desai, MD and Adela Cimic, MD
Diagnosis & Discussion
click on image for larger version
Figure 3 Figure 4 Figure 5 Figure 6 Images 1-6:
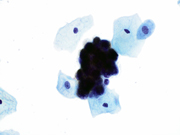
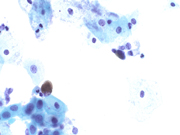
- Figure 1: ThinPrep, Papanicolaou Stain, 600x
- Figure 2: ThinPrep, Papanicolaou Stain, 600x
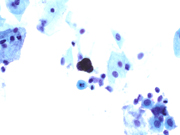
- Figure 3: ThinPrep, Papanicolaou Stain, 600x
- Figure 4: ThinPrep, Papanicolaou Stain, 600x
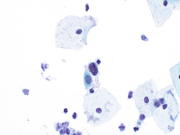
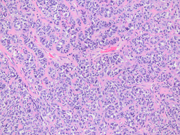
- Figure 5: A) Resection with cervico-vaginal junction. Hematoxylin and Eosin (H&E) Stain 100X B) Pigmented cells, 400x
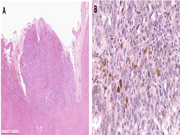
- Figure 6: Cervical PEComa. Hematoxylin and Eosin (H&E) Stain 200x
Questions:
- Based on the Pap test what is the most appropriate interpretation?
- Negative for intraepithelial lesion or malignancy (NILM)
- Atypical squamous cells of undetermined significance (ASCUS)
- Atypical squamous cells; cannot exclude high-grade squamous intraepithelial lesion (ASC-H)
- Rare cells with pigmented cytoplasm, consistent with melanoma
- Pigmented neoplastic cells in the gynecologic tract may be seen in:
- Leiomyoma and Perivascular epithelioid cell tumor (PEComa)
- Leiomyosarcoma and Serous carcinoma
- Perivascular epithelioid cell tumor (PEComa)
- Perivascular epithelioid cell tumor (PEComa) and melanoma
- Melanoma and leiomyosarcoma
Answers:
Question 1: Correct answer is DPrimary cervical vaginal melanoma is a rare tumor with ~ 60 reported cases (1). It has a poor prognosis, in part to presentation at a later/higher stage (1). The reported cytomorphologic features are variable, and the diagnosis can be overlooked due to its rarity and if amelanocytic. Rare studies have described Pap test cytomorphologic features of cervical and vaginal melanoma. Some tumors are cellular with prominent tumor diathesis while others, like this case, are paucicellular. Tumors can be epithelioid or spindle cell variant. Cells are present singly or as clusters often with high nuclear-to-cytoplasmic ratio and focally prominent nuclei. When present, melanin pigment is pathognomonic. The tumors are positive for melanocytic markers—S100, HMB45, Melan-A, SOX10 and Microphthalmia Transcription Factor (MITF).
The resection specimen confirmed the diagnosis of melanoma arising at the cervicovaginal junction (Figure 5). In contrast to cutaneous melanomas, mucosal melanomas show low mutation burden without a UV signature. Somatic mutations like SF3B1, KIT, ATRX, TP53, ARID2, SETD2 and BRAF present in cutaneous melanoma are almost never seen in mucosal melanoma.
Question 2: Correct answer is D
The major differential diagnosis of cervical vaginal melanoma is perivascular epithelioid cell tumor (PEComa).
PEComa belongs to a family of tumors derived from neural crest stem cells capable of both myoid and melanocytic differentiation (Figure 6) (2). There are two subtypes—conventional and TFE3 translocation-associated. Like melanoma, PEComa can be composed of epithelioid and spindle cells and have melanin pigment—pronounced in some cases; the cytoplasm is clear to eosinophilic and granular.
PEComa is positive for at least one melanocytic marker (e.g., HMB45, Melan-A). Unlike melanoma, it is also positive for a smooth muscle marker [e.g., SMA (most common), desmin and H-caldesmon]. S100 protein is expressed in only minority of cases and may serve as a differentiating marker from melanoma. Additionally, Cathepsin K is positive in all conventional PEComas (3).
Diagnosis of rare entities in the Pap test is challenging. The Pap test, developed for screening of squamous lesions, focuses primarily on morphologic features and less commonly use of ancillary studies, such as immunohistochemistry or molecular tests (other than detection of HPV). The most common tumors in the Pap test are adenocarcinomas of endometrial origin. Awareness of other potential entities [e.g., metastatic tumors (most commonly of breast origin) and rarely malignant melanoma, PEComa, hematologic malignancy] can aid in their recognition (4).REFERENCES
- Setia N, Goulart RA, Leiman G, Otis CN, Modem R, Pantanowtiz L. Cytomorphology of cervicovaginal melanoma: ThinPrep versus conventional Papanicolaou tests. Cytojournal. 2010 Dec 31;7:25. doi: 10.4103/1742-6413.75666. PMID: 21298024; PMCID: PMC3030001.
- WHO Classification - Female Genital Tumours (5th ed.; modified gynecology specific criteria)
- Bennett JA, Braga AC, Pinto A, Van de Vijver K, Cornejo K, Pesci A, Zhang L, Morales-Oyarvide V, Kiyokawa T, Zannoni GF, Carlson J, Slavik T, Tornos C, Antonescu CR, Oliva E. Uterine PEComas: A Morphologic, Immunohistochemical, and Molecular Analysis of 32 Tumors. Am J Surg Pathol. 2018 Oct;42(10):1370-1383. doi:
10.1097/PAS.0000000000001119. PMID: 30001237; PMCID: PMC6133752.
- Khalbuss WE, Pantanowitz L, Monaco SE. Cytomorphology of unusual primary tumors in the Pap test. Cytojournal. 2013 Aug 30;10:17. doi: 10.4103/1742-6413.117356. PMID: 24082913; PMCID: PMC3779403.