Case of the Month ...
A 69-year-old male presented to the emergency department with shortness of breath and cough. Imaging showed multiple pulmonary lung nodules, soft tissue nodularity along the right pleura, and right pleural effusion. The pleural fluid was submitted for cytologic evaluation.
Authors
Zhe Zhu, Natasha Singh, Anjali Saqi - Columbia University Irving Medical Center
Diagnosis & Discussion
click on image for larger version
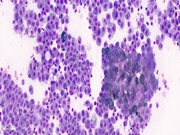
Figure 3 Figure 4 Figure 5 Images 1-5:
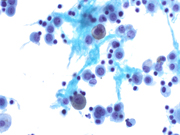
- Figure 1: Diff-Quik stain, 400x
- Figure 2: Thin-Prep 400x
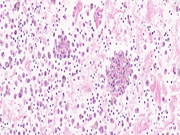
- Figure 3: Cell block 400x
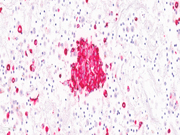
- Figure 4: HMB45 400x
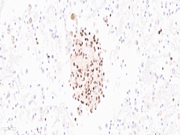
- Figure 5: SOX10 600x
Questions:
- What is the best diagnosis based on the cytomorphology in Figures 1, 2 and 3?
- Reactive mesothelial cells
- Reactive mesothelial cells with hemorrhage
- Benign, mostly histiocytes
- Adenocarcinoma
- Melanoma
- The most common risk factor(s) for this process include:
- Cirrhosis
- Congestive heart failure
- Infection
- Smoking
- Dark skin tone
Answers:
Question 1: Correct answer is EThe specimen consisted of loosely cohesive and singly dispersed epithelioid neoplastic cells with fine cytoplasmic pigment and inconspicuous-to-pinpoint nucleoli in the background of mesothelial cells and histocytes. The neoplastic cells stained with S100, HMB45, Melan-A, SOX-10, tyrosinase and PRAME. (Figures 4 and 5) The scattered mesothelial cells were highlighted by calretinin, CK5, WT1 and the numerous histiocytes by CD163 and PU1+. The clinical history (see below), cytomorphology and immunocytochemical findings were consistent with melanoma.
Question 2: Correct answer is E
The patient had a history of metastatic acral melanoma (AM) initially diagnosed ~3 years prior. AM is a rare subtype of melanoma comprising 1–3% of all melanomas and ~ 2,000–3,000 cases diagnosed annually in the United States (1). It is more common in people with darker skin tones, such as African Americans, Asians, and Hispanics, and in adults between the ages of 60 to 70 (2). Additional risk factors include pressure, friction, irritation, and inflammation (3).
Melanoma can spread via lymphatic routes, hematogenously, or direct extravascular migration to nearby or more distant sites (4). Therefore, metastases may occur in a variety of locations, including regional lymph nodes, skin, deep soft tissues, and visceral organs such as lung, liver, and brain.
AM is an aggressive malignancy with a growing prevalence (1-5). Although early detection and excision offer a potential cure, recurrences and metastases are not uncommon. Pleural effusion is an uncommon presentation of metastatic melanoma, reported in ~ 2% of all metastatic cases (6). To the best of our knowledge, this is the first report of AM in a pleural effusion.
Cytologic material containing melanoma is generally obtained from recurrent and/or metastatic tumors. The cytologic features of metastatic melanoma have been investigated in previous studies. In addition to the cytomorphology of this case, melanoma can present with large, pleomorphic epithelioid cells with occasional intranuclear cytoplasmic invaginations (pseudo-inclusions), prominent nucleoli and without cytoplasmic pigment (5). The tumor cells often exhibit staining for the above-described markers. Depending on the cytomorphology, the differential diagnosis may also include lymphoma and carcinoma. Clinical history, melanin pigment and immunocytochemical stains aid in the diagnosis.REFERENCES
- Carvalho L, Aguiar F, Smalley K, Possik P. Acral melanoma: new insights into the immune and genomic landscape. Neoplasia. 2023; 46:100947.
- Bradford P, Goldstein A, McMaster M, Tucker M. Acral lentiginous melanoma: incidence and survival patterns in the United States, 1986-2005. Arch Dermatol. 2009;145(4):427-34.
- Lee J, Choi Y, Hwang J, et al. Frequency of Trauma, Physical Stress, and Occupation in Acral Melanoma: Analysis of 313 Acral Melanoma Patients in Korea. Ann Dermatol. 2021; 33(3): 228–236.
- Ubellacker J, Tasdogan A, Ramesh V, et al. Lymph protects metastasizing melanoma cells from ferroptosis. Nature. 2020; 585(7823):113-118.
- Mejbel H, Torres-Cabala C, Milton D, et al. Prognostic significance of acral lentiginous histologic type in T1 melanoma. Mod Pathol. 2021; 34(3):572-583.
- Sumalani K, Rehman U, Akhter N, Rizvi N. Black pleural effusion: an unusual presentation of metastatic melanoma diagnosed by medical thoracoscopy. Respirol Case Rep. 2019; 7(9): e00490.