Case of the Month ...

A 68-year-old male presented with a 7.8 cm anterior mediastinal mass with intense radiotracer uptake on PET/CT imaging, concerning for lymphoma or other malignancy. The patient has a history of Hodgkin’s lymphoma initially diagnosed in 2023, status post chemotherapy. He subsequently underwent endobronchial ultrasound evaluation of the mediastinal mass with performance of fine needle aspiration and core needle biopsy.
Authors
- Daisy Sun, MD PhD, Miami Valley Hospital, Dayton, OH
- Kyle Wang, The Seven Hills School, Cincinnati, OH
Diagnosis & Discussion
click on image for larger version
Figure 3 Figure 4 Figure 5 Figure 6 Images 1-6:
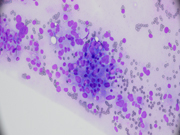
- Figure 1: Rapid on-site evaluation (ROSE) FNA material of mediastinal mass, smear, Diff-Quik stain, x 40 maginification
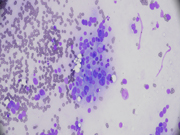
- Figure 2: Rapid on-site evaluation (ROSE) FNA material of mediastinal mass, smear, Diff-Quik stain, x 400 maginification
- Figure 3: Rapid on-site evaluation (ROSE) FNA material of mediastinal mass, smear, Diff-Quik stain, x 400 maginification
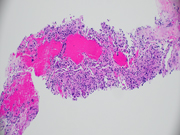
- Figure 4: Core biopsy of mediastinal mass, H&E, x 100 magnification
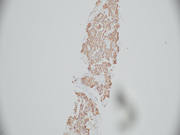
- Figure 5: Core biopsy of mediastinal mass, chromogranin, x 100 magnification
- Figure 6: Core biopsy of mediastinal mass, S100, x 100 magnification
Questions:
- What is the best diagnosis based on the cytomorphology, histomorphology and immunohistochemical findings in Figures 1 through 6?
- Paraganglioma
- Neuroendocrine tumor
- Melanoma
- Granular cell tumor
- Adenocarcinoma
- How do you differentiate malignant from benign paragangliomas?
- Cytological atypia
- Metastasis
- Binucleation and pseudoinclusion
- Size > 5 cm
- Mitotic rate >10 per 10 high power fields
- The strongest genetic risk factor for developing metastatic paraganglioma is which of the following?
- NF1
- RET oncogene
- SDHB mutations
- THEM127
- VHL
Answers:
Question 1: Correct answer is A
The smears (Figs 1-3) show a hypercellular specimen with cells in clusters or singly, displaying marked pleomorphism and abundant delicate granular cytoplasm. Core biopsy material (Fig 4) shows tumor cells arranged in a trabecular or nested pattern, separated by a rich microvasculature. Performed IHC shows the tumor cells are positive for chromogranin (Fig 5), synaptophysin, and INSM1. They are negative for AE1/3, TTF-1, PTH, and thyroglobulin. S100 (Fig 6) highlights sustentacular cells. The Ki-67 was <3% and SDHB showed intact cytoplasmic staining. In all, the combined cytomorphologic, histologic and immunohistochemical findings are most consistent with paraganglioma, given the zellballen pattern of tumor cell arrangement separated by thin fibrovascular septae that contain S100-positive sustentacular cells.
Paragangliomas may share a fair amount of morphologic and immunohistochemical overlap with neuroendocrine tumors; however, neuroendocrine tumors lack sustentacular cells. Additionally, neuroendocrine tumors are generally positive for cytokeratin, whereas paragangliomas are cytokeratin negative. Both melanomas and granular cell tumors may consist of large epithelioid cells with abundant eosinophilic cytoplasm; however, both of these tumors are S100 positive and generally lack any significant staining with markers of neuroendocrine differentiated and cytokeratins. Granular cell tumors also co-express the histocytic marker CD68. Melanomas will generally be SOX10 positive as well as positive for at least one marker of melanoma differentiation, such as HMB45, Melan-A, or PRAME. Unlike paragangliomas, adenocarcinomas are generally cytokeratin positive, lack diffuse expression of more than one neuroendocrine marker, and do not have a sustentacular framework.Question 2: Correct answer is B
Anterior mediastinal masses can be a significant diagnostic challenge. The well-known 4T’s commonly seen in the anterior mediastinum are thymoma, teratoma, thyroid tissue, and “terrible” lymphoma. Paragangliomas (PGs) are extra-adrenal pheochromocytomas and account for < 0.3% of mediastinal masses. Most mediastinal PGs originate from the posterior region, though these tumors can arise in the anterior and middle mediastinum.
PGs originate from a diffuse neuroendocrine system from the skull base to the pelvic floor and preferentially arise along the sympathetic chain in the thorax, abdomen, and pelvis or along the parasympathetic chain in the head and neck, with occurrence in the head and neck region most common. As mentioned, these tumors can be sympathetic or parasympathetic and functional (i.e. catecholamine producing) or nonfunctional. PGs can be sporadic or arise in association with hereditary syndromes, like multiple endocrine neoplasia type 2 (MEN2), neurofibromatosis type 1 (NF1), von Hippel Lindau (VHL), etc.
PGs can behave biologically benign or malignant. Malignant PGs are rare and diagnosis of malignant PGs requires evidence of metastasis at nonchromaffin sites distant from the primary tumor. Malignant behavior cannot be predicted based on morphologic or immunohistochemical features alone.Question 3: Correct answer is C
The rate of malignancy is higher in hereditary PGs than in sporadically arising tumors. The strongest genetic risk factor for the development of metastasis in the clinical context of a PG diagnosis is identification of a germline SDHB mutation. SHDB mutated PGs are currently associated with the most aggressive clinical presentation, clinical course, and rate of death from disease.