Case of the Month ...

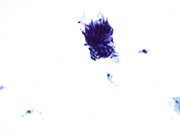
A 45-year-old obese female, with recent diagnoses of pelvic inflammatory disease. Gynecologic history is significant for 5 years of abnormal pap smears with no follow-up, colposcopy or LEEP. The physical examination appeared normal. No vaginal bleeding or postcoital bleeding was reported. Fluid-based cytology sample was obtained and analyzed using Roche Cobas Assay for high risk HPV (human papilloma virus). Results were positive for HPV 16 DNA. ThinPrep Pap test from endocervix was examined.
Authors
- Yodsuí Figueroa Hernández, MD; Adela Cimic, MD. Department of Pathology and Cell Biology. Columbia University Irving Medical Center. New York Presbyterian Hospital, New York, NY.
click on image for larger version
Figure 3 Figure 4 Figure 5 Figure 6 Images 1-6:
- Figure 1: Pap test, endocervix, ThinPrep: 400x magnification
- Figure 2: Pap test, endocervix, ThinPrep: 400x magnification
- Figure 3: Pap test, endocervix, ThinPrep: 400x magnification
- Figure 4: Cell block, Hematoxylin and Eosin (H&E) stain: 400x magnification
- Figure 5: Cell block, p16 immunohistochemical stain, 400x magnification
- Figure 6: Cell block, ki-67 immunohistochemical stain, 400x magnification
Questions:
Based on the ThinPrep slide, cell block cytomorphology and immunohistochemical stains (Figure 1 to 9), what is the best diagnosis?
- High-grade intraepithelial malignancy
- Small cell neuroendocrine carcinoma
- Adenocarcinoma in situ (AIS)
- Adenocarcinoma
- What are the criteria for reporting Adenocarcinoma in situ (AIS) on a Pap test?
- Cells occurring in sheets and strips, with nuclear enlargement, hyperchromasia, crowding, overlap and/or pseudostratification, coarse chromatin, occasional mitoses and/or apoptotic bodies, cell groups resembling rosettes/glands or feathering
- Increased nuclear-to-cytoplasmic ratio, salt-pepper chromatin, nuclear molding and necrosis
- Small, round, blue single cells with tingible bodies macrophages and lymphoglandular bodies
- Two-toned cytoplasm, normal nuclear size, prominent nucleoli, intracytoplasmic vacuoles
- What is the next step in management for Adenocarcinoma in situ?
- Follow-up Pap test in 6 months
- Loop Electrosurgical Excision Procedure (LEEP)
- Hysterectomy
- Colposcopy with endocervical sampling
- What is the next step in management for Adenocarcinoma in situ?
- Follow-up Pap test in 6 months
- Loop Electrosurgical Excision Procedure (LEEP)
- Hysterectomy
- Colposcopy with endocervical sampling
Answers:
Question 1: Correct answer is C - Adenocarcinoma in situ (AIS).
Adenocarcinoma in situ is often associated with high risk human papilloma virus 16 and 18 (hr HPV 16, 18). The morphologic examination of the Pap test is commonly sufficient for interpretation. However, if feasble, creation of a cell block for immunohistochemistry performance with p16 and Ki67 may aid in rendering the diagnosis. P16 functions as an inhibitor of cyclin-dependent kinases through Integration of high risk HPV into host-cell DNA via persistent infection, resulting in retinoblastoma (RB) protein inactivationand degradation by E7 leading to RB pathway negative feedback inducing overexpression of p16. The overexpression of p16has been used as a surrogate marker for premalignant and malignant cervical lesions. HPV E6 proteins interact with multiple host proteins including the E3-ligase, E6AP, which is also known as UBE3A. Recruitment of E6AP by HPV16 (16E6) forms a destruction complex that promotes p53 degradation through E6AP-mediated polyubiquitination, leading to uncontrolled cell proliferation and tumorigenesis. HPV E6 oncoproteins also alter numerous other cellular processes, such as DNA damage repair, cell signaling, and gene expression, which contribute to their oncogenic properties.Per the 2014 update to TheBethesda System, the cytomorphologic features of adenocarcinoma in situ include the above-listed features. The cytomorphologic features listed in Answer B are seen in small cell carcinoma. The fetures listed in Answer C are seen in lymphocyte-rich processes, such as high-grade lymphomas. The features in Answer D are seen in radiation-induced cellular injury.
Question 2: Correct answer is A - Cells occurring in sheets and strips, with nuclear enlargement, hyperchromasia, crowding, overlap and/or pseudostratification, coarse chromatin, occasional mitoses and/or apoptotic bodies, cell groups resembling rosettes/glands or feathering.
Question 3: Correct answer is D - Colposcopy with endocervical sampling.Based on the latest guidelines from the American Society for Colposcopy and Cervical Pathology, the recommended management for women diagnosed with any subcategory of AGC and adenocarcinoma in situ (AIS) entails undergoing colposcopy with endocervical sampling. This recommendation applies irrespective of human papillomavirus (HPV) test results.
Question 4: Correct answer is C - Tumor diathesis in 50% of the cases; abundant and large pleomorphic cells with granular cytoplasm, cytoplasmic vacuolization, round and hyperchromatic nuclei, loss of nuclear polarity, true nuclear crowding, prominent nucleoli. Cells are mostly arranged in crowded sheets, clusters and isolated cells.
The cytomorphologic features of adenocarcinoma typically appreciable on liquid-based cytology Pap tests include pleomorphic to columnar cells with granular cytoplasm, cytoplasmic vacuolization, loss of nuclear polarity, true nuclear crowding, nuclei with clumped chromatin, marked variation of nucleoli, occasional mitotic figures, and presence of abundant blood. Adenocarcinomas of the cervix associated with HPV infection represent 85 - 90% of all adenocarcinomas. Cell block and immunostains may be attempted to confirm the cytomorphologic impression.REFERENCES:
Wang T, Hua Y, Liu L, Leng B. Analysis of atypical glandular cells in ThinPrep Pap smear and follow-up histopathology. Proc (Bayl Univ Med Cent). 2024 Mar 21;37(3):403-407. doi: 10.1080/08998280.2024.2324656. PMID: 38628324; PMCID: PMC11018051
Wilbur DC. Practical issues related to uterine pathology: in situ and invasive cervical glandular lesions and their benign mimics: emphasis on cytology-histology correlation and interpretive pitfalls. Mod Pathol. 2016 Jan;29 Suppl 1:S1-11. doi: 10.1038/modpathol.2015.138. PMID: 26715169
Wang, J.C.K., Baddock, H.T., Mafi, A. et al. Structure of the p53 degradation complex from HPV16. Nat Commun 15, 1842 (2024). https://doi.org/10.1038/s41467-024-45920-w
Teoh D, Musa F, Salani R, Huh W, Jimenez E. Diagnosis and Management of Adenocarcinoma in Situ: A Society of Gynecologic Oncology Evidence-Based Review and Recommendations. Obstet Gynecol. 2020 Apr;135(4):869-878. doi: 10.1097/AOG.0000000000003761. PMID: 32168211; PMCID: PMC7098444
Sung JA, Nikas IP, Kim H, Ryu HS, Lee C. Diagnostic distribution and pitfalls of glandular abnormalities in cervical cytology: a 25-year single-center study. J Pathol Transl Med. 2022 Nov;56(6):354-360. doi: 10.4132/jptm.2022.09.05. Epub 2022 Nov 9. PMID: 36345619; PMCID: PMC9682225
Ryu A, Honma K, Shingetsu A, Tanada S, Yamamoto T, Nagata S, Kamiura S, Yamasaki T, Ohue M, Matsuura N. Utility of p16/Ki67 double immunocytochemistry for detection of cervical adenocarcinoma. Cancer Cytopathol. 2022 Dec;130(12):983-992. doi: 10.1002/cncy.22631. Epub 2022 Aug 17. PMID: 35976043
Edyta C. Pirog, Bernhard Kleter, Semra Olgac, Piotr Bobkiewicz, Jan Lindeman, Wim G.V. Quint, Ralph M. Richart, Christina Isacson. Prevalence of Human Papillomavirus DNA in Different Histological Subtypes of Cervical Adenocarcinoma. The American Journal of Pathology, Volume 157, Issue 4, 2000,
Pages 1055-1062, ISSN 0002-9440, https://doi.org/10.1016/S0002-9440(10)64619-6Lastra RR, Park KJ, Schoolmeester JK. Invasive Stratified Mucin-producing Carcinoma and Stratified Mucin-producing Intraepithelial Lesion (SMILE): 15 Cases Presenting a Spectrum of Cervical Neoplasia With Description of a Distinctive Variant of Invasive Adenocarcinoma. Am J Surg Pathol. 2016 Feb;40(2):262-9. doi: 10.1097/PAS.0000000000000543. PMID: 26523540.
Lee KR, Trainer TD. Adenocarcinoma of the uterine cervix of small intestinal type containing numerous Paneth cells. Arch Pathol Lab Med. 1990 Jul;114(7):731-3. PMID: 2363632.
Fujiwara K, Monk B, Devouassoux-Shisheboran M. Adenocarcinoma of the uterine cervix: why is it different? Curr Oncol Rep. 2014 Dec;16(12):416. doi: 10.1007/s11912-014-0416-y. PMID: 25325935.
Stolnicu S, Barsan I, Hoang L, Patel P, Terinte C, Pesci A, Aviel-Ronen S, Kiyokawa T, Alvarado-Cabrero I, Pike MC, Oliva E, Park KJ, Soslow RA. International Endocervical Adenocarcinoma Criteria and Classification (IECC): A New Pathogenetic Classification for Invasive Adenocarcinomas of the Endocervix. Am J Surg Pathol. 2018 Feb;42(2):214-226. doi: 10.1097/PAS.0000000000000986. PMID: 29135516; PMCID: PMC5762258.